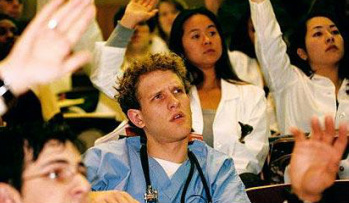
Despite that they look younger and younger with each passing year (to those of us getting older and older), medical residents are clearly adults. But are they “adult learners”? Should we treat them as such? This interesting question was raised at the Society for Education in Anesthesia Meeting– a meeting dedicated to educational theory and best ways to teach the next generations of anesthesiologists. Even more interesting, the question was broached by a resident!
The father of the “adult learner” theory is Malcolm Knowles, who said: “The adult’s self-concept of self-directivity is in direct conflict with the traditional practice of the teacher telling the students what they need to learn.”
Most modern theories of adult learning application are centered around themes in that quote – the need for adults to be autonomous, direct their own learning, select their own learning goals, and understand (and presumably agree with) the reasons why they should learn something. (Of course, this concept is not embraced by all).
If our task is to educate the next generation of doctors, it is really appropriate to have the learners decide what bits of information they think is important to learn? Do we not have a responsibility to society to ensure that they emerge from our training programs as fully educated, competent physicians? Of course, the Accreditation Council of Graduate Medical Education believes so, and that’s the reason this Society for Education in Anesthesia meeting is focused on the development and measurement of “milestones” , which the ACGME defines as “competency-based developmental outcome expectations that can be demonstrated progressively by residents and fellows from the beginning of their education through graduation to the unsupervised practice of their specialty.”
Will our efforts to find educational activities that are well-received by the millennial generation eventually sabotage us by failing to produce new doctors who have truly learned what they need to learn? And in this hyper age of information and technology, how can we decide what information is actually needed at the ready, in their minds, and what they can simply know they should look up.
What’s your take?







